X-Ray Safety Toolkit
Canada Safe Imaging | Radiation Safety Institute of Canada
What is Canada Safe Imaging and how does it relate to the Bonn Call for Action?
Ten main actions are identified as being essential for the strengthening of radiation protection in medicine over the next decade. The actions are not listed in order of importance:
Action 1: Enhance the implementation of the principle of justification
Action 2: Enhance the implementation of the principle of optimization of protection and safety
Action 3: Strengthen manufacturers’ role in contributing to the overall safety regime
Action 4: Strengthen radiation protection education and training of health professionals
Action 5: Shape and promote a strategic research agenda for radiation protection in medicine
Action 6: Increase availability of improved global information on medical exposures and occupational exposures in medicine
Action 7: Improve prevention of medical radiation incidents and accidents
Action 8: Strengthen radiation safety culture in health care
Action 9: Foster an improved radiation benefit-risk-dialogue
Action 10: Strengthen the implementation of safety requirements globally
Canada Safe Imaging has been formed to address the call in this country.
Bonn Call for Action
World Health Organization
- https://www.who.int/publications/m/item/bonn-call-for-action
- https://www.who.int/ionizing_radiation/medical_exposure/Bonn_call_action.pdf
- https://www.who.int/teams/environment-climate-change-and-health/radiation-and-health/medical-exposure/bonn-call-for-action
International Atomic Energy Agency (IAEA)
- https://www.iaea.org/resources/rpop/resources/bonn-call-for-action-platform
- https://www.iaea.org/sites/default/files/17/12/bonn-call-for-action.pdf
International Society of Radiographers and Radiological Technologists
Toolkit Purpose
- over half the respondents were not aware of the Bonn Call to Action;
- radiation safety iniatives are inconsisently implemented and followed across medical fields in Canada;
- there is a lack of eduation and training in radiation safety; and
- there is a need to engage all stakeholders;
They conclude with the following statement:
Solutions may require a collaborative approach involving all stakeholders in radiation protection. Based on the findings of this survey, these solutions will likely include, but not be limited to, education and training, and the development and regular review of regulations and guidelines.
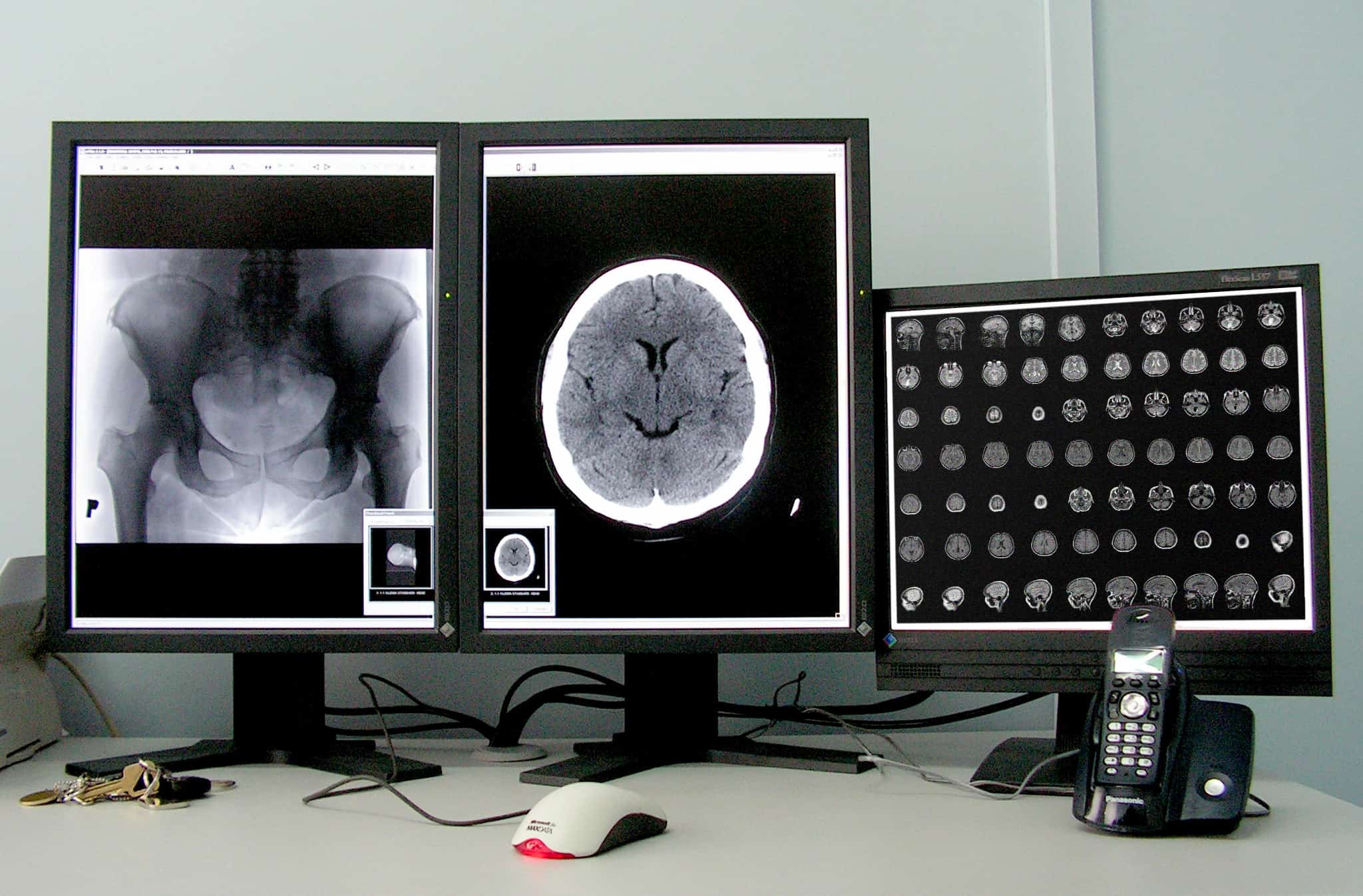
This toolkit has been developed to consolidate resources for radiation safety in medical imaging applications into one location. While it is focused on x-ray safety, it also includes information related to radionuclides as they are used as biomarkers or tags in imaging studies which may also include x-ray.
Global Safe Imaging Initiatives

Ionizing Radiation in Medical Imaging
X-Ray
CT
Nuclear Medicine Tracers

PPE, Dosimetry, & Radiation Protection
 Radiation safety dose limits for workers are clearly defined in legislation. This is not the case for doses obtained for medical purposes. It is up to the medical practitioner to balance the benefits of using ionizing radiation for the purposes of diagnosis and/or treatment and the increased risk of adverse effects.
Radiation safety dose limits for workers are clearly defined in legislation. This is not the case for doses obtained for medical purposes. It is up to the medical practitioner to balance the benefits of using ionizing radiation for the purposes of diagnosis and/or treatment and the increased risk of adverse effects.
The effects of ionizing radiation on a cell, tissue, organ or human, depends on how much energy is absorbed into it. A dose of radiation is a measure of how much energy is given to the body from radiation and the effect it may have. There are 3 common ways dose is reported: absorbed dose, which is the energy given to the body by radiation per unit mass, measured in gray; equivalent dose, which also takes the type of radiation into account, measured in sieverts; and effective dose, which additionally considers the sensitivity of different tissues to radiation, which is also measured in sieverts. A gray or a sievert would be a very large dose. More typically doses would be on the scale of 1/1000 (milli-) or 1/1000000 (micro-) of the base unit. In radiation safety practice it is assumed that for chronic exposures of low dose radiation, there is an increased risk of developing a fatal cancer of 4% per 1000 mSv dose, over and above the 25% natural fatal cancer risk. In their 2017 Report on Occupational Exposures in Canada, Health Canada found the mean effective dose for those being monitored for radiation exposure in a medical setting during 2016 was 0.07 mSv. Removing all those who received zero dose, the average was 0.55 mSv. This demonstrates that even with a full career in the medical sector, by following proper health and safety protocols, worker doses can be kept low.
The situation for patients is different in that there is no offical record of their lifetime accumulated dose due to medical interventions. The paper, “Effective Doses in Radiology and Diagnostic Nuclear Medicine: A Catalog” compiles over 25 years of studies on medical doses of ionizing radiation. With respect to medical imaging, the authors state, “standard radiographic examinations have average effective doses that vary by over a factor of 1000. Computed tomographic examinations tend to be in a more narrow range but have relatively high average effective doses (approximately 2–20 mSv) [.] Average effective dose for most nuclear medicine procedures varies between 0.3 and 20 mSv. These doses can be compared with the average annual effective dose from [natural] background radiation of about 3 mSv.”
While it is up to the medical practitioner to determine what is in the best interest of the patient, exposure to ionizing radiation in the medical workplace is regulated provincially/territorially in the case of most x-rays and federally in the case of nuclear medicine. Dosimeters are used to track worker dose, which PPE is worn to minimize worker (and patient) exposure.
We have no senses to detect ionizing radiation. Exposure can lead to health consequences that appear days or years later, depending upon the strength of the dose, the tissue receiving it, and the type of damage incurred. For this reason, dosimetry is used to determine how much energy radiation has deposited into an individual. If exposures get too high, actions must be taken. The type of dosimetry program used depends upon the type of radiation expected to be encountered and the part of the body expected to receive it. A dosimetry program for external exposures would be different than that for internal exposures. If both types of exposures might be expected, then both programs would be needed.
X-ray radiation is best shielded with dense materials such as lead or tungsten. Designs of radiography rooms include shielding considerations, and portable shielding such as lead aprons or screens are utilized. Nuclear medicine tracers may require plastic shielding or a combination of plastic and a more-dense material. PPE for x-ray functions mainly to absorb the energy of the radiation before it interacts with living tissue. PPE for nuclear medicine also needs to prevent contact with radioative tracers.
PPE & Dosimetry are only two components of a full radiation safety program and not the first step. Higher-level aspects which should be in place before ionizing radiation sources are in use are having qualified and trained staff, implementing the As Low As Reasonably Achievable (ALARA) principle, the development and implementation of radiological controls and standard operating procedures with the intent of keeping doses ALARA, the development and training of staff on emergency procedures which consider mulitple contingencies, following required recordkeeping and reporting requirements, and setting up internal audit procedures.

Associations & Regulations by Jurisdiction

Alberta
Associations
Relevant Acts and Regulations
Provincial OHS
Additional Resource

British Columbia
Associations
Relevant Acts and Regulations
Provincial OHS
Accreditation
Additional Resource

Manitoba
Relevant Acts and Regulations
Provincial OHS

New Brunswick
Relevant Acts and Regulations
Provincial OHS

Newfoundland & Labrador
Relevant Acts and Regulations
Provincial OHS

Northwest Territories
Associations
Contact us to let us know the details of medical imaging associations in the Northwest Territories.
Relevant Acts and Regulations
Nova Scotia
Associations
Relevant Acts and Regulations
Health Protection Act, SNS 2004, c 4
Medical Imaging and Radiation Therapy Professionals Act, SNS 2013, c 7
Occupational Health and Safety Act, SNS 1996, c 7
Occupational Safety General Regulations, S.N.S. 1996, c. 7
Workers’ Compensation Act, SNS 1994-95, c 10
Workers’ Compensation General Regulations, NS Reg 22/96 Amended 167/20
Provincial OHS
Additional Resource
Nunavut
Associations
Contact us to let us know the details of medical imaging associations in Nunavut.
Relevant Acts and Regulations

Ontario
Associations
Relevant Acts and Regulations
Provincial OHS
- Ontario – Ministry of Labour – Health & Safety
- Ontario – Ministry of Labour – Radiation Hazards & Protection
Sector-Based Health & Safety Associations:
- Infrastructure Health & Safety Association
- Public Services Health & Safety Association
- Workplace Safety & Prevention Services
- Workplace Safety North
Cross-Sector Health & Safety Associations:

Prince Edward Island
Relevant Acts and Regulations
Provincial OHS

Québec
l'Associations
Lois et Règlements Pertinents

Saskatchewan
Relevant Acts and Regulations
Provincial OHS
Quality Assurance
Additional Resource

Yukon
Associations
Contact us to let us know the details of medical imaging associations in the Yukon.
Relevant Acts and Regulations
Territorial OHS

Federal X-Ray
Associations
- Alliance of Medical Radiation and Imaging Technologists Regulators of Canada
- Canadian Association of Medical Radiation Technologists
- Canadian Association of Radiologists
- Canadian College of Physicists in Medicine
- Canadian Organization of Medical Physicists
- Canadian Heads of Academic Radiology
- Canadian Radiation Protection Association
- Canadian Radiological Foundation
- Canadian Society for Breast Imaging
- Canadian Society for Interventional Radiology
Relevant Acts & Regulations
- Canada Labour Code (Federally-Regulated Workplaces)
- Radiation Emitting Devices Act
Federal OHS
Health Canada Safety Codes
- Safety Code 30: Radiation Protection in Dentistry
- Safety Code 35: Safety Procedures for the Installation, Use and Control of X-ray Equipment in Large Medical Radiological Facilities
- Safety Code 36: Radiation Protection and Quality Standards in Mammography – Safety Procedures for the Installation, Use and Control of Mammographic X-ray Equipment

Nuclear Medicine
Associations
Relevant Acts and Regulations

Training & Education

External Resource Links
Canada Safe Imaging Member Sites
- Canadian Association of Medical Radiation Technologists
- Canadian Association of Nuclear Medicine
- Canadian Association of Radiologists
- Canadian College of Physicists in Medicine
- Canada Health Infoway
- Canadian Organization of Medical Physicists
- CECR (Centre d’expertise clinique en radioprotection)
- Choosing Wisely
- Medtech – Canada’s Medical Technology Companies
- Ontario Association of Medical Radiation Sciences (OAMRS)
- Radiation Safety Institute of Canada
International Organizations - Medical Imaging
Medical Imaging Radiation Safety Sites & Publications of Interest
- Canadian Agency for Drugs and Technologies in Health – Issues in Emerging Health Technologies; Clinical Decision Support Systems for Diagnostic Imaging
- Canadian Agency for Drugs and Technologies in Health – Canadian Medical Imaging Inventory
- Canadian Association of Radiologists Journal
- Canadian Centre for Occupational Health & Safety – Radiation – Quanitities and Units of Ionizing Radiation
- Canadian Health Infoway
- Canadian Medical Devices Directorate
- CAR Diagnostic Imaging Referral Guidelines
- Centre d’Expertise Clinique en Radioprotection
- Choosing Wisely Canada
- COMP Report: A Survey of Radiation Safety Regulations for Medical Imaging X-Ray Equipment in Canada (2020)
- Health Council of Canada – Decisions, Decisions: Family Doctors as Gatekeepers to Prescription Drugs and Diagnostic Imaging in Canada (2010)
- IAEA – Radiation Protection of Patients
- IAEA – Radiation Protection of Pregnant Women in Radiology
- ICRP Publication 103 – The 2007 Recommendations of the International Commission on Radiological Protection
- ICRP Publication 113 – Education and Training in Radiological Protection for Diagnostic and Interventional Procedures
- ICRP Publication 121 – Radiological Protection in Paediatric Diagnostic and Interventional Radiology
- ICRP Publication 128 – Radiation Dose to Patients from Radiopharmaceuticals: A Compendium of Current Information Related to Frequently Used Substances
- ICRP Publication 129 – Radiological Protection in Cone Beam Computed Tomography (CBCT)
- ICRP Publication 135 – Diagnostic Reference Levels in Medical Imaging
- ICRP – Radiation and Your Patient – A Guide for Medical Practitioners
- Image of Care (CAMRT)
- Journal of Clinical Orthopaedics and Trauma – Radiation Protection and Standardization (2018)
- Mayo Clinic Proceedings – Concise Review for Clinicians – Radiation Risk from Medicial Imaging (2010)
- The Medical Imaging Team
- Najjar R (July 10, 2023) Radiology’s Ionising Radiation Paradox: Weighing the Indispensable Against the Detrimental in Medical Imaging. Cureus 15(7): e41623. doi:10.7759/cureus.41623
- National Research Council – Tracking Radiation Exposure from Medical Diagnostic Procedures: Workshop Report (2012)
- Radiology Info – General Nuclear Medicine
- Therapeutic Products Directorate
- World Health Organization Quality Systems for Medical Imaging: Guidelines for Implementation and Monitoring
National & International Resources - PET/CT
CNSC
- Radionuclide Information Booklet
- GD-52: Design Guide for Nuclear Substance Laboratories and Nuclear Medicine Rooms
- REGDOC-1.4.1 Licence Application Guide: Class II Nuclear Facilities and Prescribed Equipment
- REGDOC-1.5.1, Version 1.1 Application Guide: Certification of Radiation Devices or Class II Prescribed Equipment
- REGDOC-1.6.1 Version 2 Licence Application Guide: Nuclear Substances and Radiation Devices
- REGDOC-1.6.2 Developing and Implementing an Effective Radiation Protection Program for Nuclear Substances and Radiation Devices Licences
- Type II Inspection Worksheet Use Type: 862 – Diagnostic Nuclear Medicine Procedures
IAEA
- IAEA Safety Standards
- PET/CT Training Material
- Radiation Protection in Newer Medical Imaging Techniques: PET/CT
- Radiation Protection During PET/CT
- Radiation Protection of Children During PET/CT
- Radiation Protection of Patients During PET/CT Scanning
- Radiation Protection of Pregnant Women During PET/CT Scanning
- Radiation Protection of Staff During PET/CT Scanning
- Strategies for Clinical Implementation and Quality Management of PET Tracers
- Hermanne, A., Tárkányi, F. T., Ignatyuk, A. V., Takács, S., & Capote, R. (2021). Upgrade of IAEA recommended data of selected nuclear reactions for production of PET and SPECT isotopes. Nuclear Data Sheets, 173, 285–308.
IAEA Human Health Series
- No. 1 – Quality Assurance for PET and PET/CT Systems
- No. 9 – Appropriate Use of FDG-PET for the Management of Cancer Patients
- No. 11 – Planning a Clinical PET Centre
- No. 26 – Standard Operating Procedures for PET/CT: A Practical Approach for Use in Adult Oncology
- No. 27 – PET/CT Atlas on Quality Control and Image Artefacts
- No. 32 – Clinical PET/CT Atlas: A Casebook of Imaging in Oncology
- No. 37 – Nuclear Medicine Resources Manual 2020 Edition
IAEA Pocket Guides
- For Medical Physicists Supporting Response to a Nuclear or Radiological Emergency
- Medical Management of Persons Internally Contaminated with Radionuclides in a Nuclear or Radiological Emergency
IAEA Radioisotopes and Radiopharmaceuticals Reports
- No. 1 – Emerging Positron Emitters for Medical Applications: 64Cu and 124I
- No. 3 – Guidance on Facility Design and Production of [18F]Fluorodeoxyglucose (FDG)
IAEA-TECDOC
- 1430 – Radioisotope handling facilities and automation of radioisotope production
- 1603 – The Role of PET/CT in Radiation Treatment Planning for Cancer Patient Treatment
- 1605 – A Guide to Clinical PET in Oncology: Improving Clinical Management of Cancer Patients
IAEA Technical Report Series
- No. 468 – Cyclotron Produced Radionuclides: Physical Characteristics and Production Methods
- No. 471 – Cyclotron Produced Radionuclides: Guidelines for Setting Up a Facility
ICRP
Related Health Canada Publications
- An Inexpensive Medical X-Ray Image Quality Control Test Tool
- Canadian Computed Tomography Survey – National Diagnostic Reference Levels
- Canadian Mammography Quality Guidelines
- Diagnostic X-Ray Imaging Quality Assurance: An Overview
- Independent Test Specifications for Dosimetry Services: X-Radiation
- It’s Your Health – Whole Body Screeging Using MRI or CT Technology
- Modernization of the Radiation Emitting Devices Act (REDA) 2020 Consultation – Summary of Results
- Occupational Radiation Exposures in Canada
Related CNSC Publications (Nuclear Medicine)
- Nuclear Medicine Infographic
- Medical Imaging and Radiotherapy Infographic
- Diagnostic Imaging and Ionizing Radiation Infographic
General Information
Other Pages Related to Nuclear Medicine
- Class II Facilities and Prescribed Equipment Forms
- Document History of REGDOC-2.5.6, Design of Rooms Where Unsealed Nuclear Substances Are Handled
- Event Reporting: Class II Nuclear Facilities
- Event Reporting: Nuclear Medicine
- Nuclear Facilities: Nuclear Substance Processing
- Nuclear Substances
- Nuclear Substances and Radiation Devices Forms
- Nuclear Substances and Radiation Devices Mentorship Program
- Waste Management
General Radiation Safety Sites & Publications
- Canadian Radiation Protection Association
- Health Physics Society
- International Agency for Research on Cancer
- International Atomic Energy Agency
- International Commission on Radiological Protection
- Inter-Agency Committee on Radiation Safety
- International Radiation Protection Association
- National Council on Radiation Protection and Measurements
- National Research Council. 2006. Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2. Washington, DC: The National Academies Press.
- Occupational Radiation Protection Networks
- United Nations Scientific Committee on the Effects of Atomic Radiation
- World Health Organization



